A Guide to Hormone Suppression Therapy: Your Path to Healing and Survivorship
- Qudus Wix specialist
- Jul 26
- 18 min read
If you're reading this, chances are your life, or the life of someone you love, has been touched by a cancer diagnosis. I get it. When you’re first thrown into this world, you’re hit with a flood of new information and intimidating terms. Hormone suppression therapy is often one of them, a critical part of the plan for those with hormone-positive breast cancer.
This guide is meant to be a warm, reassuring hand to hold as we walk through what it all means—translating the medical jargon into clear, comforting knowledge. This is a journey of healing, and you have the strength to navigate it. We’re in this together.
Your Journey with Hormone Therapy Starts Here
Facing a cancer diagnosis can feel like you’ve been dropped in a foreign country with a map you can’t read. Words like "hormone receptor-positive" or "endocrine therapy" sound so clinical and intimidating.
But let’s break it down with a sense of hope. Think of it this way: certain breast cancer cells need a specific type of "fuel" to grow. For many, that fuel is a hormone, like estrogen or progesterone. This is what we call hormone-positive cancer.
Hormone suppression therapy is simply a brilliant strategy to cut off that fuel supply. It’s a targeted treatment designed to slow or even stop the growth of these cancers, giving your body the upper hand. This isn't about brute force; it's a smart, calculated approach to protect you, a vital step in your survivorship.
What It Means to Be Hormone Receptor-Positive vs. Negative
When you get your pathology report back after a biopsy or surgery, you’ll likely see terms like ER-positive (ER+) or PR-positive (PR+). I know it looks like medical code, but seeing a "+" here is actually good news.
It tells your oncology team that the cancer cells have receptors—picture them as tiny, open docking stations—for estrogen (ER) or progesterone (PR).
This information is incredibly valuable. It means the cancer has a clear vulnerability, a weak spot that we can target with specific, effective treatments. It unlocks a whole pathway for your care, giving you a powerful tool in your fight.
For about two out of every three breast cancers, these receptors are present. This means for the majority of women, hormone therapy becomes a cornerstone of their treatment and survivorship plan. If your cancer is hormone-negative (ER-/PR-), it means it doesn't use these hormones to grow, and your team will focus on other effective treatments like chemotherapy.
Before we dive deeper, let's quickly summarize what these key ideas mean for you and your treatment journey.
Hormone Suppression Therapy at a Glance
This table offers a quick summary of the key concepts to help you understand your treatment journey.
Key Concept | What It Means For You |
|---|---|
Hormone Receptor-Positive (ER+/PR+) | Your cancer has a "fuel source" (estrogen/progesterone) that can be targeted, opening the door for effective treatment and a more personalized fight. |
Targeted Treatment | Instead of a broad approach, this therapy specifically targets the cancer cells' ability to grow. It's a strategic move for your health. |
Reducing Recurrence Risk | A primary goal is to lower the chances of cancer returning, giving you more peace of mind and confidence in your future. |
Long-Term Ally | This therapy is often taken for 5-10 years, acting as a long-term partner and a daily act of commitment to your survivorship. |
Understanding these basics is the first step toward feeling more in control and less overwhelmed.
Setting a Hopeful Path Forward
This journey is about so much more than just medical appointments and pills. It's about finding your footing again and reclaiming your sense of hope. Knowing why you’re taking a certain treatment is the first step toward feeling empowered. This guide is your roadmap, designed to help you see hormone therapy not as a burden, but as a long-term ally in your health.
Here’s what this all boils down to for you:
A Personalized Plan: Your treatment is tailored specifically to your cancer's biology, not a one-size-fits-all approach.
A Focus on Prevention: A huge part of hormone therapy is to dramatically reduce the chances of recurrence, helping you look toward the future with more confidence.
Empowered Participation: When you understand the "why," you can be an active, confident partner in your own care. You're not just a passenger on this ride.
Throughout this guide, we'll explore everything from how these therapies work to managing side effects with practical, real-life strategies. You are starting a journey toward healing, and you absolutely have the strength to navigate it with grace and grit. You are not alone.
How Hormone Therapy Fights Cancer

To really feel in control of your treatment, it helps to get what’s actually happening inside your body. So, let’s pull back the curtain on hormone suppression therapy, but without the dense medical jargon. It’s a beautifully simple idea, and understanding it can be incredibly empowering.
Think of your hormones, especially estrogen and progesterone, as a set of keys. For certain breast cancers—the ones we call hormone receptor-positive (HR+)—the cancer cells have developed special locks on their surface, known as receptors. When the right hormone "key" fits into the cancer cell's "lock," it sends a crystal-clear signal: "Grow and multiply!"
Hormone suppression therapy is like bringing in a master locksmith. It uses two main strategies to stop these cancer cells in their tracks, which is what makes it a game-changer for anyone with an HR+ diagnosis.
Blocking the Cancer Cell's Receptors
The first approach is to cleverly block the locks. This is where drugs like Tamoxifen come in. It’s part of a class of medications called Selective Estrogen Receptor Modulators, or SERMs. Think of a SERM as a key that fits perfectly into the cancer cell's lock but is designed not to turn.
It just sits there, jamming the lock. When the real estrogen key comes along, it can’t get in because the space is already taken. The cancer cell never gets the message to grow, which effectively starves it of its instructions.
This is a powerful way to stop cancer growth without totally overhauling the amount of estrogen in your system. It just prevents the hormone from doing its damage where it matters most—at the site of the cancer cells.
By blocking these growth signals right at the source, hormone therapy doesn't just treat the cancer; it actively works to prevent it from coming back. This is why it's so often a long-term part of a survivorship plan.
For so many women, taking this pill is a daily act of self-care and a real commitment to a healthier future. It’s your shield, working quietly in the background every single day.
Lowering the Body's Hormone Levels
The second strategy is simply to reduce the number of keys. This method focuses on lowering the total amount of estrogen your body produces. For women who have gone through menopause, most estrogen isn't made in the ovaries anymore; it’s produced in body fat by an enzyme called aromatase.
This is where Aromatase Inhibitors (AIs) enter the picture. Medications like Letrozole or Anastrozole work by blocking that aromatase enzyme. In doing so, they drastically cut down on estrogen production, leaving far fewer "keys" available to unlock any cancer cells that might be hanging around.
For premenopausal women, a similar result can be achieved through what’s called Ovarian Function Suppression (OFS). This treatment uses medication or, in some cases, surgery to temporarily or permanently stop the ovaries from making estrogen. Since the ovaries are the main estrogen factory before menopause, this shuts off the fuel supply for the cancer.
Why It Only Works for HR+ Cancers
This brings us to a really crucial point: why hormone suppression therapy is a lifeline for HR+ cancers but isn't used for hormone receptor-negative (HR-) cancers.
It’s pretty straightforward. If a cancer is HR-negative, its cells just don't have those special "locks" for estrogen or progesterone. Trying to use hormone therapy would be like trying to unlock a door that has no keyhole.
Hormone Receptor-Positive (HR+): The cancer cells have receptors (the locks) and use hormones (the keys) to grow. Hormone therapy works because it can either block the locks or get rid of the keys.
Hormone Receptor-Negative (HR-): The cancer cells don't have these receptors. They're fuelled by different signals, so blocking hormones wouldn't have any effect on their growth. Other treatments like chemotherapy are used for these cancers.
This difference really shows how personalized cancer care has become. Your treatment is specifically designed to target your cancer's unique biology, giving you the most effective path forward. Understanding this "why" can transform your daily medication from a simple pill into a powerful, strategic tool in your wellness arsenal.
Understanding Your Treatment Plan and Timeline
Your treatment plan isn’t a one-size-fits-all prescription; it’s a strategy built just for you. When you and your oncology team land on hormone suppression therapy, you're creating a personalized roadmap based on your unique biology, whether you're pre- or post-menopausal, and what you want for your long-term health. Committing to this for five or even ten years can feel like a lot, but I want you to reframe it: this is your powerful, proactive way of fighting for a long and healthy future.
Starting a long-term treatment can feel overwhelming, but knowing what to expect can turn that uncertainty into a feeling of control. Let's walk through the main types of therapies and how your team figures out the right path for your journey.
The Main Types of Hormone Therapy
Think of your treatment options like a specialized toolkit. Your medical team will pick the right tool for the job based on one key factor: whether your ovaries are still producing estrogen (premenopausal) or have stopped (postmenopausal).
The three main players in this toolkit are:
Tamoxifen: This is often the first choice for premenopausal women, but it can also be used by women who are postmenopausal. It works by sitting on the estrogen receptors of cancer cells, essentially blocking the "key" (estrogen) from getting into the "lock" and telling the cell to grow.
Aromatase Inhibitors (AIs): This group of drugs, which includes letrozole and anastrozole, is typically for postmenopausal women. They work by blocking an enzyme called aromatase, which stops the body from making estrogen in other places like body fat after the ovaries have shut down.
Ovarian Function Suppression (OFS): For premenopausal women, this treatment puts the ovaries on a temporary or permanent pause, shutting down the body’s main estrogen factory. It’s often used together with Tamoxifen or an AI to create an even stronger hormonal blockade.
Making the call on which path to take is a huge step, and it can feel heavy. For a much deeper, personal look into this process, you might find our guide on [navigating the hormone therapy decision after breast cancer](https://www.gracegritandpinkribbons.com/post/hormone-therapy-after-breast-cancer-decision) really helpful.
The image below shows some of the key benefits you can get by sticking with your personalized hormone therapy plan.
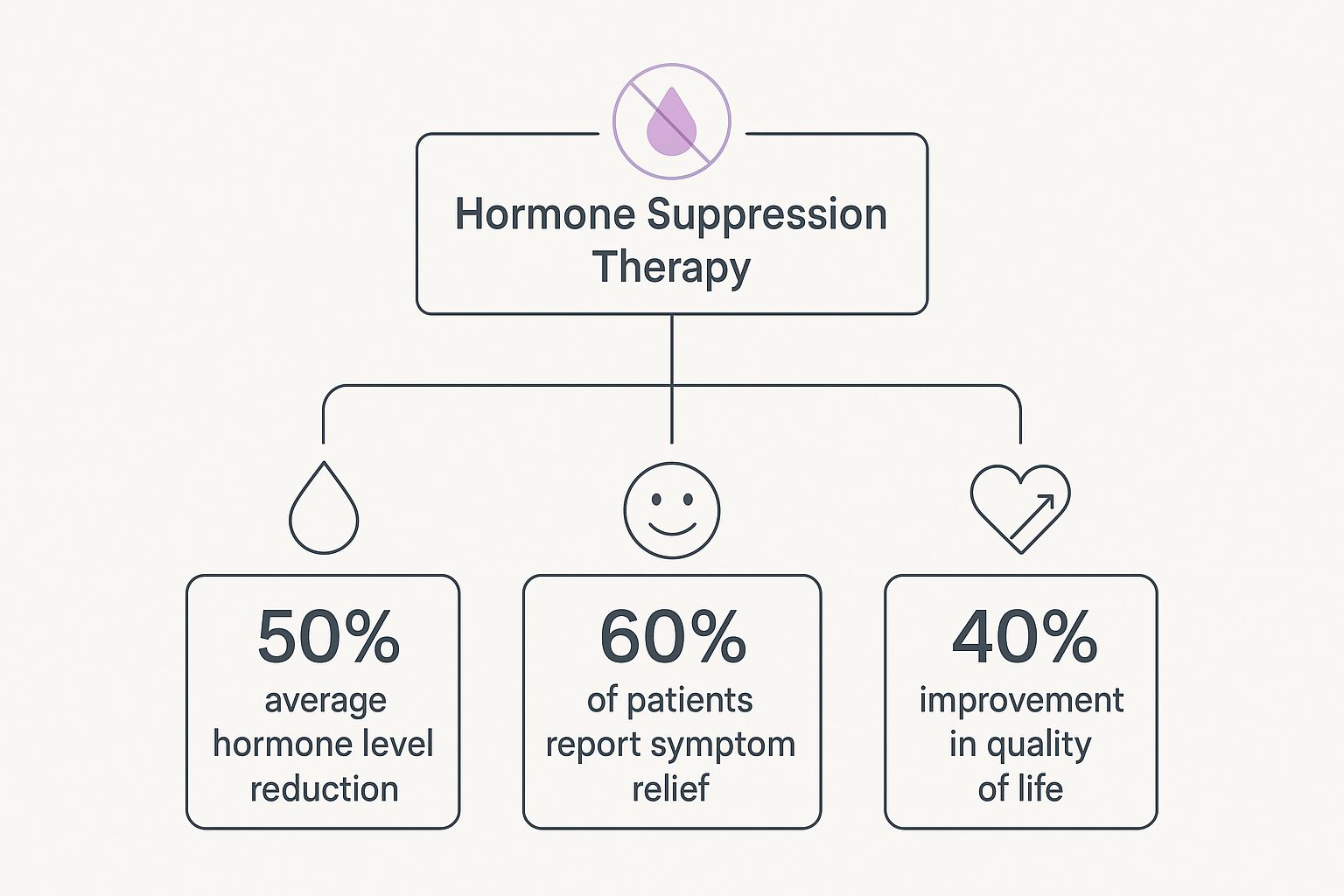
It’s a good reminder of how effective these treatments can be, not just in fighting cancer but in helping many of us feel better and manage symptoms.
Staying the Course for Long-Term Health
Committing to a daily pill for five or ten years takes real dedication, but it’s one of the most powerful things you can do to lower your risk of the cancer coming back. This long-term commitment is your shield, actively protecting you long after the initial, intense treatments are over. Being consistent is everything; staying on track with your medication gives it the best possible chance to work.
Your journey with hormone therapy is a marathon, not a sprint. Try to frame that daily pill not as a chore, but as an act of self-love—a promise you're making to your future self. It’s one small step, every single day, toward a life with more peace and less fear.
Each day you take your medication is another win in your survivorship story. It's proof of your resilience and your commitment to your own health. You’ve got this.
How to Manage Side Effects with Practical Care

Let's have a real, honest chat. Choosing hormone suppression therapy is a huge act of self-preservation. It’s a commitment to your future, and that takes incredible strength. But we also have to be real about the day-to-day: this journey can bring its own set of challenges. Side effects are common, and they aren't just a footnote in your treatment plan—they're a part of your daily life.
You might be in the middle of a work meeting when a sudden wave of heat takes over (hello, hot flashes), or you might wake up with stiff, achy joints and a bone-deep tiredness that no amount of coffee can fix. These experiences are real, they are valid, and you don’t have to just "power through" them.
Think of this section as your personal toolkit for navigating these side effects with grace, grit, and a healthy dose of practical care. You are the CEO of your own well-being. You have the power to make small, daily decisions that protect your quality of life and help you feel more like yourself. You're in the driver's seat.
Your Toolkit for Common Side Effects
Dealing with side effects isn't about finding one magic bullet. It's about creating a multi-layered, proactive approach. It's the small, consistent actions that add up to make a huge difference over time. Let's break down some of the most common hurdles and how you can face them head-on.
Taming Hot Flashes
These sudden, intense waves of heat can be disruptive and, frankly, embarrassing. But you have options.
Dress in Layers: This is your new superpower. Being able to quickly shed a cardigan or scarf when a flash hits can bring instant relief.
Identify Your Triggers: Grab a small notebook and, for a week, jot down when your hot flashes strike. You might start seeing a pattern connected to spicy foods, caffeine, alcohol, or even stress.
Cooling Strategies: A small fan on your desk or by your bed is a game-changer. A cooling pillow or a light spritz of water on your face can also work wonders in the moment.
Soothing Joint Pain and Stiffness
That feeling of waking up like the Tin Man before he found his oil can? That's a very common complaint, often caused by the drop in estrogen.
Get Moving Gently: I know it sounds counterintuitive when you're sore, but movement is medicine. Gentle activities like walking, swimming, or yoga help lubricate your joints and ease the pain. Even 15-20 minutes a day makes a difference.
Stay Hydrated: Water helps keep cartilage soft and supple. Make it a habit to sip water consistently throughout the day.
Consider Complementary Therapies: Many women find incredible relief from acupuncture. Studies have shown it can be very effective for the joint pain that comes with Aromatase Inhibitors.
Remember, you are an active participant in your care. Your voice matters. If a side effect is truly impacting your life, speak up. Your oncology team has heard it all and can offer medical solutions, from trying a different medication to prescribing low-dose antidepressants that help with both hot flashes and mood.
Embracing Lifestyle and Nutritional Support
What you eat and how you move are two of the most powerful tools in your arsenal. This isn’t about perfection; it’s about nourishing your body with intention and kindness.
For a deeper dive, check out our complete guide to [living well and thriving despite hormone therapy side effects](https://www.gracegritandpinkribbons.com/post/living-well-with-hormone-therapy-side-effects-your-empowering-guide).
To get you started, here are a few practical strategies for some of the most common side effects.
Practical Strategies for Common Side Effects
This table breaks down some actionable tips to help you feel more in control.
Common Side Effect | Nutritional Tip | Lifestyle Strategy |
|---|---|---|
Fatigue | Focus on balanced meals with protein, healthy fats, and complex carbs to stabilize energy. Avoid sugar crashes. | Schedule short rest periods. A 20-minute nap can be more restorative than pushing through exhaustion. |
Mood Swings | Incorporate omega-3 fatty acids from sources like salmon and walnuts, which support brain health and mood regulation. | Practice mindfulness or meditation for 5-10 minutes a day to calm your nervous system and create emotional space. |
Vaginal Dryness | Stay well-hydrated. Talk to your doctor about non-hormonal moisturizers and lubricants made specifically for this purpose. | Gentle pelvic floor exercises can increase blood flow to the area, which can help with tissue health. |
Every small, positive choice you make is a victory. It's a declaration that you are more than your diagnosis, more than your treatment, and that you are dedicated to living a full, vibrant life.
Using Food to Feel Strong and Resilient
Food is one of the most powerful—and joyful—tools you have in your corner, especially when you’re navigating hormone suppression therapy. I want to be clear: this isn’t about strict diets or meals that suck the joy out of eating. It’s about finding a delicious, nourishing way of eating that actually supports your body, helps ease some of those tough side effects, and makes you feel more vibrant and strong.
Think of your body like it’s running a marathon. It needs premium fuel to stay strong, fight that bone-deep fatigue, and protect itself for the long road ahead. Making mindful food choices is a small act of kindness you can do for yourself every single day. It's a way to take back a little bit of control and be an active participant in your own healing.
Leaning Into a Plant-Forward Plate
Shifting to a more plant-forward way of eating can be a real game-changer during and after cancer treatment. This doesn't mean you have to go full-on vegetarian or vegan (unless you want to!). It simply means making a conscious choice to fill your plate with more foods that grow from the earth.
Picture a colourful plate piled high with leafy greens, bright berries, crunchy veggies, and whole grains. These foods are absolutely packed with phytochemicals and antioxidants—think of them as your body’s personal security team, helping to protect your cells from damage.
Some key foods to invite onto your plate include:
Cruciferous Veggies: Things like broccoli, cauliflower, and kale are rich in compounds that support healthy cell function.
Berries and Dark Fruits: Blueberries, raspberries, and cherries are antioxidant powerhouses that can help fight inflammation.
Legumes and Beans: Chickpeas, lentils, and black beans are fantastic sources of fibre and plant-based protein for steady, sustained energy.
Whole Grains: Oats, quinoa, and brown rice offer fibre to support your digestive system and B vitamins to help combat that crushing fatigue.
When you focus on these foods, you’re not just eating; you’re strategically giving your body what it needs to be resilient.
Protecting Your Bones and Heart
Some hormone therapies, especially Aromatase Inhibitors (AIs), can cause bone thinning over time. This makes looking after your bone health a top priority. Your bones are literally the framework that holds you up, and keeping them strong is non-negotiable for your long-term well-being.
Calcium and Vitamin D are the ultimate dynamic duo for bone health. Calcium is the building block, and Vitamin D is like the key that unlocks the door, letting your body absorb that calcium.
Definitely talk to your oncology team about what you need specifically. They might recommend supplements, but you can also get a lot from your food. Good sources of calcium include dairy, fortified plant milks, leafy greens like kale, and sardines. For Vitamin D, think fatty fish like salmon, fortified foods, and a little bit of safe sun exposure.
It’s also so important to think about your heart. These therapies can affect your cardiovascular health risks down the line. Research shows a clear link between some hormone therapies and an increased risk of cardiovascular disease (CVD) in cancer survivors. To learn more, check out studies on cardiovascular risk in cancer survivors on ahajournals.org. Protecting your heart through diet and exercise is a vital part of your long-term wellness plan.
Eating to Ease Those Side Effects
Smart food choices can also be your best friend when it comes to managing those all-too-common side effects. Fighting fatigue? It starts with keeping your blood sugar stable. Instead of reaching for a sugary snack that will just lead to a crash, try balanced mini-meals with protein, healthy fats, and fibre to keep your energy steady.
And for that awful joint pain, focus on anti-inflammatory foods. Turmeric, ginger, walnuts, and fatty fish are all great choices. A warm mug of golden milk (turmeric mixed with a plant-based milk) can be a really soothing and delicious daily ritual.
Eating well on this journey is an act of deep self-respect. It’s you, telling yourself that you are worthy of care, nourishment, and feeling the best you possibly can.
Thriving in Survivorship and Your New Normal

Ringing the bell after finishing chemo or radiation is a huge deal. It’s a moment you’ve been dreaming of, a chance to finally take a deep breath. But the truth is, the healing journey doesn't stop there. For many of us on long-term hormone suppression therapy, this is where a new chapter truly begins—the one about survivorship and figuring out what our "new normal" actually looks like.
This phase is a messy, beautiful mix of feelings. There’s so much gratitude for still being here, but there's also that quiet hum of anxiety that gets a little louder before every check-up. We call it "scanxiety." Then there’s the fear of recurrence, which can creep in at the most unexpected times. These feelings are real, and they are completely valid parts of living with cancer and becoming a survivor.
The goal isn't to pretend these feelings don't exist, but to learn how to live alongside them. This is your time to redefine what life looks like now, to seek out joy, and to build a life that feels rich and full. It’s not just about surviving anymore; it’s about learning how to thrive with a strength you never knew you had and a deeper appreciation for every single day.
Rediscovering Yourself After Cancer
Cancer changes you. There’s no way around it. A big part of this journey is giving yourself the grace to get to know the person you are now. Your priorities might have shifted completely. Your whole perspective on life is likely much deeper. This is your chance to get reacquainted with this new version of yourself.
Survivorship is an active, ongoing process of healing. It’s about more than just staying cancer-free; it's about intentionally creating a life filled with purpose, connection, and joy, even amidst the uncertainties.
Embracing this new normal means figuring out what lights you up again. Maybe it’s an old hobby you let slide, that art class you’ve always wanted to take, or simply spending more quiet moments in nature. For a deeper dive into this, check out our [guide to thriving with cancer wellness](https://www.gracegritandpinkribbons.com/post/your-guide-to-thriving-with-cancer-wellness).
This long-term commitment to your health is what survivorship is all about. Sticking with your prescribed hormone therapy is one of the most impactful things you can do for your future. The evidence is clear: for hormone-positive cancers, staying on therapy for the recommended duration significantly lowers the risk of recurrence and improves overall survival. It is a powerful commitment to your long-term health.
Building Your Supportive Community
You had a whole team with you during treatment, and you don’t have to walk through survivorship alone either. Finding your people—the ones who just get it without you having to explain—is one of the most powerful things you can do for yourself.
Seek Out Support Groups: Connecting with other women on hormone therapy, whether it’s online or in person, can be so incredibly validating.
Lean on Loved Ones: Be open with your friends and family about what you actually need. Sometimes, all you need is someone to listen without trying to fix anything.
Consider Professional Help: A therapist who specializes in oncology can give you invaluable tools for managing the fear and anxiety that can pop up.
Your new normal is like a blank canvas waiting for you. It’s going to be a masterpiece of resilience, filled with moments of joy, connection, and a gratitude so profound you can feel it in your bones. You've walked through fire and come out stronger. Now is the time to live fully, with all the grace and grit you've more than earned.
Your Questions, Answered
When you're dealing with something as big as hormone suppression therapy, it’s natural for questions to pop up. Big ones, small ones, and all the "what ifs" in between. Feeling curious or even a little anxious is a good sign—it means you're diving deep and taking charge of your health. Think of this as a conversation about the practical and emotional questions that come up along the way.
Will Hormone Suppression Therapy Put Me Into Menopause?
This is a really common question, and the answer isn't a simple yes or no. For women who are still having periods, some therapies like Tamoxifen might not stop them completely, but they can definitely bring on symptoms that feel a whole lot like menopause, such as hot flashes and fatigue.
Then there are treatments specifically designed to stop your ovaries from producing estrogen—this is called Ovarian Function Suppression (OFS). This approach will trigger a medical menopause. Depending on your specific treatment plan, this could be temporary or it might be permanent. It's so important to have a frank, open conversation with your oncology team so you know exactly what to expect.
Can I Still Have Children After Hormone Therapy?
For many younger women diagnosed with breast cancer, fertility is a massive and completely valid concern. How hormone therapy impacts your ability to have children really comes down to the specific drugs you're prescribed.
Some treatments act like a pause button on your ovarian function, and your fertility might return once you stop. Others, unfortunately, can cause permanent infertility. If having children is part of your future plans, you absolutely must bring this up with your medical team before you start therapy. They can connect you with a fertility specialist to talk about options like egg or embryo freezing, which can help preserve your ability to have a family down the road.
Planning ahead is an act of hope. Discussing fertility preservation isn't about dwelling on the negative; it's about empowering yourself with options and taking control of your future, whatever it holds.
How Do I Deal With the Emotional Side of Long-Term Treatment?
Looking after your emotional health during this marathon is just as vital as managing the physical side effects. It’s completely normal to feel a whole mix of things—gratitude that you have this treatment, anxiety about what’s next, and even frustration with the day-to-day reality of it all. This is all part of living with cancer.
Building a strong support system is your lifeline. This might look like a few different things:
Talking to a professional: A therapist who specializes in working with cancer patients can give you invaluable tools to cope.
Finding your people: Joining a support group, whether it's online or in-person, connects you with others who just get it. No explanation needed.
Practicing self-compassion: Give yourself some grace. Things like journaling, mindfulness, or even just some gentle movement can help you create space for all those feelings.
Remember, reaching out for help is a sign of incredible strength. You don't have to carry all of this on your own.
Is It Safe to Take Supplements While on Hormone Therapy?
This is a big one, and it requires a lot of caution. Your doctor will likely recommend supplements like calcium and Vitamin D to keep your bones strong, but you have to be really careful with anything else.
Many over-the-counter supplements, especially ones marketed for menopause symptoms like black cohosh or soy isoflavones, actually contain plant-based estrogens. These could potentially get in the way of your hormone suppression therapy and work against your treatment. Always, always talk to your oncologist before starting any new vitamin, supplement, or herbal remedy. They are your best and safest source of information.
At Grace Grit and Pink Ribbons, we know the journey doesn’t just stop when active treatment ends. It’s a path of rediscovery, healing, and finding your strength in community. We’re here to walk alongside you with resources and encouragement that come straight from the heart. Find your sanctuary and connect with others who understand at https://www.gracegritandpinkribbons.com.





Comments