A Hopeful Guide to Navigating Triple Positive Breast Cancer
- Qudus Wix specialist
- Jul 27
- 17 min read
Getting a triple-positive breast cancer diagnosis can feel overwhelming, and the medical jargon can make your head spin. But I want you to take a breath and reframe this. This specific diagnosis isn't just a label; it’s a detailed road map. It gives your medical team three distinct "positive" signals—think of them like keys to a lock—that point directly to a highly effective, personalized treatment plan.
This isn't just a diagnosis; it's a direction. Those "positives" are known targets, and having a clear target is the first step toward a powerful victory. This is a journey you are fully equipped to handle.
What It Means to Be Triple Positive
Hearing the words "triple positive breast cancer" sounds incredibly complex, but the concept is more straightforward than you might think. In simple terms, it means the cancer cells have tested positive for three specific things that they use as fuel to grow.
Imagine three different "on" switches are stuck in the "on" position, feeding the cancer.
The inspiring part? Because we know exactly what these switches are, we have targeted therapies designed specifically to turn them off. It’s like a gardener who doesn’t just see a patch of weeds, but knows exactly which types they are and has the perfect tool to pull each one out for good. This knowledge allows for a multi-pronged attack that is tailored specifically to your cancer, giving you a powerful sense of control and hope.
Understanding Your Three Positives
So, what are these three “positives”? They refer to specific receptors found on the surface of the cancer cells. You can think of receptors as tiny docking stations. When the right signal—in this case, a hormone or a growth factor—docks onto the receptor, it tells the cell to grow and divide.
Estrogen Receptor Positive (ER+): This means the cancer is Hormone Positive. The cells have docking stations for the hormone estrogen. When estrogen latches on, it fuels the cancer's growth.
Progesterone Receptor Positive (PR+): In the same way, the cells also have docking stations for the hormone progesterone, another fuel source, reinforcing its Hormone Positive status.
HER2 Positive (HER2+): The cells are making way too much of a protein called Human Epidermal growth factor Receptor 2. This overproduction of HER2 sends a constant, aggressive signal for the cells to grow and multiply uncontrollably.
Here’s a simple table to break it down.
Understanding Your Three Positives
The 'Positive' Receptor | What It Means | How It Guides Treatment |
|---|---|---|
Estrogen Receptor (ER+) | The cancer uses the hormone estrogen as fuel to grow. | We can use hormone-blocking drugs (like Tamoxifen or aromatase inhibitors) to cut off this fuel supply. |
Progesterone Receptor (PR+) | The cancer also uses the hormone progesterone as a fuel source. | Hormone-blocking therapies also work to block this pathway, often alongside targeting estrogen. |
HER2 (HER2+) | The cancer cells make too much of the HER2 protein, causing aggressive growth. | We can use targeted therapies (like Herceptin or Perjeta) that specifically find and block the HER2 protein. |
Having these three known drivers means your treatment can be incredibly strategic, targeting each pathway for a more powerful, combined effect.
This infographic helps visualize how the three components come together.
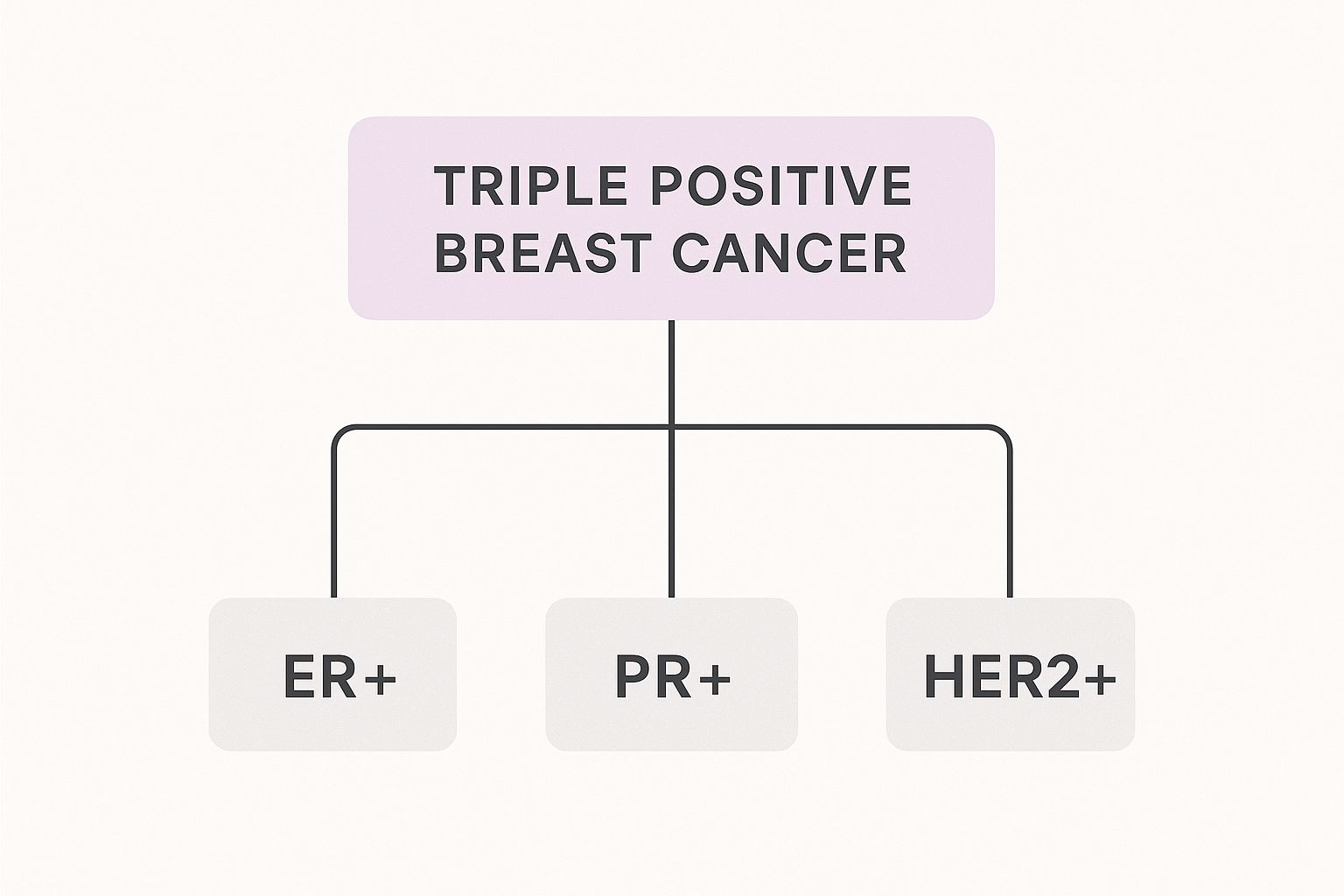
As the diagram shows, a triple-positive diagnosis isn't just one thing. It's a combination of three distinct factors, and each one gives us a clear path to attack the cancer.
A Roadmap for Treatment
Having these three clear targets is incredibly empowering. It means your treatment won't be a generic, one-size-fits-all approach. Instead, your doctors can layer different therapies—hormone blockers for ER/PR and targeted drugs for HER2—to shut down every growth signal. This strategic combination is why this diagnosis often leads to very positive outcomes.
Of course, a clear path doesn't mean the journey is the same for everyone. Outcomes can be heavily influenced by other factors, especially access to care. For example, in the Caribbean, where the breast cancer incidence rate is around 50.2 cases per 100,000 women, outcomes are often impacted by limited access to the very targeted therapies that make treatment for triple-positive cancer so effective. The high cost and low availability of crucial treatments like anti-HER2 therapies and hormone blockers can unfortunately create major barriers and affect survival rates. You can explore more about these regional healthcare disparities and their impact on breast cancer outcomes to better understand the global picture.
How Doctors Pinpoint Your Diagnosis and Stage
The time between finding a lump and getting a clear answer can feel like an eternity. It's often filled with a storm of "what-ifs" and a level of anxiety that’s hard to describe. But this diagnostic phase isn't just about waiting—it’s where your medical team becomes a team of detectives, piecing together every clue to build your personalized game plan.
Think of it like this: your team is creating a detailed instruction manual for your specific cancer. Once they have that manual, they know exactly how to dismantle it. This is where your power begins—with knowledge.
The First Steps: Imaging and Biopsy
For most of us, the journey starts with imaging tests. A mammogram gives a foundational X-ray of the breast tissue. If something looks suspicious, an ultrasound often comes next, using sound waves to get a better look and help figure out if a lump is a solid mass or just a fluid-filled cyst.
If those scans show something that needs a closer look, the next, most crucial step is a biopsy. A biopsy is the only way to know for certain if cancer is present. It sounds intimidating, but it’s a procedure where a specialist carefully removes a small tissue sample from the area. This is the moment that provides the concrete answers needed to move forward.
"When the doctor said, ‘I’m sorry to tell you this, but it’s breast cancer,’ I was like, ‘What do you mean?’... I left the office with all these cards and papers and was just thinking, Whose life is this? This is crazy.” - Tiffany Kinkead, diagnosed at 26.
That initial shock is a feeling so many of us share—a moment where life seems to hit the pause button. But it’s also the moment the fight truly begins, armed with the information that comes next.
Unlocking the Code: Your Pathology Report
That tiny piece of tissue from the biopsy is sent to a pathologist, a specialist who analyzes it under a microscope. Their findings are put into a pathology report, which is probably the single most important document in your diagnosis. It’s not just a verdict; it’s your cancer’s blueprint.
This report confirms not just that it’s cancer, but exactly what kind of cancer it is. To get a triple positive breast cancer diagnosis, the pathologist runs specific tests looking for those three key receptors.
ER/PR Testing: They use a special staining process called immunohistochemistry (IHC). You can think of it like a dye that only sticks to estrogen and progesterone receptors. If the cells change colour, it’s a “positive” result, confirming the cancer is Hormone Positive.
HER2 Testing: The IHC test is also used for HER2. If the result is unclear or borderline, a more precise test called FISH (fluorescence in situ hybridization) is used. The FISH test actually counts the number of HER2 genes in the cancer cells, giving a very clear yes-or-no answer.
This detailed analysis tells your team exactly which "on" switches are active, confirming the ER+, PR+, and HER2+ status that defines your path forward.
Demystifying Cancer Staging
Once the type of cancer is confirmed, the next piece of the puzzle is staging. The word "staging" can sound terrifying, but it's important to understand what it really means. Staging isn't a judgment on how "bad" your cancer is; it’s simply a map that tells your doctors about the cancer's size and location.
It really just answers three basic questions:
How large is the main tumour?
Has it spread to any nearby lymph nodes?
Has it spread (metastasized) to distant parts of the body?
The stages, numbered from 0 to IV, give doctors a universal way to describe the cancer's extent. Stage 0 is non-invasive. Stages I-III describe invasive cancers that are still within the breast or have only spread to nearby lymph nodes. Stage IV, also known as metastatic breast cancer, means the cancer has travelled to other organs.
Knowing the stage is fundamental. It helps determine whether your treatment will focus on local therapies (like surgery and radiation) or if it needs to include systemic therapies (like chemo, hormone therapy, and targeted drugs) that travel throughout the body to fight cancer wherever it might be. This information is the final piece needed to build a powerful, effective, and deeply personal treatment strategy just for you.
Your Personalized Triple-Threat Treatment Plan

When you receive a triple positive breast cancer diagnosis, it feels like everything is spinning out of control. But what this diagnosis really gives your medical team is a detailed playbook—a clear road map for how to fight back. This isn't a one-size-fits-all battle; it’s a strategic, coordinated attack where every move is designed for the unique biology of your cancer.
Think of it as having a three-pronged strategy. The cancer has three known vulnerabilities, and your doctors have three powerful types of treatment ready to take on each one. It's this multi-faceted approach that makes the outlook so hopeful. Let's break down this powerful treatment team.
Smart Missiles Targeting HER2
First up is tackling that overactive HER2 protein. The therapies for this are a true marvel of modern medicine.
Imagine these treatments as heat-seeking missiles programmed to find one thing and one thing only: the HER2 receptors on your cancer cells. Drugs like trastuzumab (Herceptin) and pertuzumab (Perjeta) are antibodies that literally hunt down and latch onto these receptors.
Once they dock, they do a couple of incredible things:
They shut down the "grow and divide" signal that the HER2 protein is constantly sending.
They act like a giant flare, flagging the cancer cell for destruction by your own immune system.
This targeted approach is incredibly effective, and because it leaves most healthy cells alone, it often comes with fewer side effects than traditional chemo. It’s a precision strike aimed right at the cancer's engine.
Cutting Off the Fuel Supply with Hormone Therapy
Next in your treatment arsenal is hormone therapy, sometimes called endocrine therapy. This powerful strategy goes after the Hormone Positive (ER+ and PR+) side of your cancer.
If HER2 drugs are the smart missiles, think of hormone therapy as cutting off the enemy's fuel lines. Since these cancer cells feast on estrogen and progesterone to grow, these medications work by either slashing your body's hormone levels or physically blocking hormones from feeding the cancer cells.
For many of us, this means taking a daily pill like tamoxifen or an aromatase inhibitor (like letrozole or anastrozole). This is a long-term commitment, often for five to ten years, but it's one of the most crucial parts of your plan to reduce the risk of recurrence. The side effects of hormone therapy can be challenging, but they are manageable, and connecting with others on a similar path can provide invaluable support and practical tips.
"Because we had a plan, we stuck to it, I counted down, I checked things off, and we got it done... Even though I lost my hair, and I stopped working, I got through it and felt like I had checked that box off and was done." - Stacy, diagnosed with Stage 1 Triple Positive Breast Cancer.
Having a clear, actionable plan can turn that overwhelming fear into focused determination, empowering you to take on each step of your survivorship journey.
The Strategic Role of Chemotherapy
Finally, there’s chemotherapy. For many women with triple positive breast cancer, chemo acts as the heavy-duty "clean-up crew."
While targeted and hormone therapies are incredibly precise, chemotherapy is a systemic treatment that goes after any fast-growing cells throughout your body. It’s often used before surgery (neoadjuvant chemo) to shrink the tumour and make it easier to remove, or after surgery (adjuvant chemo) to hunt down any microscopic cancer cells that may have escaped.
The thought of chemo can be scary. We all know about the side effects like fatigue and hair loss. But for an aggressive cancer, it plays a vital strategic role. It's the broad-spectrum part of your plan that ensures every last trace is dealt with. Remember, every side effect has a solution, and your healthcare team is there to help you manage them with strength and grace.
Your personalized plan will layer these three treatments—HER2-targeted therapy, hormone therapy, and chemotherapy—in a specific sequence to give you the best possible outcome. Each one has a distinct job, and together, they create a formidable force, giving you multiple, powerful ways to reclaim your health and thrive.
Nourishing Your Body Through Treatment

Going through treatment for triple positive breast cancer is one of the most demanding projects your body will ever undertake. Good nutrition isn't just another chore to add to your list—it's your essential supply line. Think of food as a profound act of self-care, a way to build back your strength, and a powerful tool to regain a sense of control when so much feels overwhelming.
This isn’t about strict diets or a long list of forbidden foods. It's about making small, thoughtful choices that add up to a big difference in how you feel, day in and day out. You are literally fuelling your body for the incredible work it’s doing to heal.
Managing Common Side Effects with Food
Treatment side effects are real, but so are the strategies to manage them. When you understand why certain foods can help, you can build your own “food-as-medicine” toolkit to navigate the ups and downs. Let's walk through some of the most common hurdles and see how your plate can help you clear them.
This simple, nourishing approach can be a lifeline, especially in regions where access to advanced care is a challenge. Take the Caribbean, for example, where breast cancer is the most common cancer among women. Survival rates can be deeply affected by late diagnoses and limited access to the targeted therapies used for triple positive breast cancer.
With five-year survival rates between 24% and 38% in some of these areas, focusing on supportive care like nutrition becomes an even more critical part of a patient's resilience and overall well-being. You can read more about the regional realities of breast cancer in the Caribbean to better understand these dynamics.
Your body is working overtime to heal. Honour that hard work by giving it the best possible fuel. Every nourishing bite is a small victory, a quiet way of saying, "I am on my own side."
This proactive approach to nutrition helps you become a partner to your medical team, supporting your body from the inside as the treatments do their work on the outside.
Your Food-as-Medicine Toolkit for Side Effects
Think of this table as your go-to cheat sheet for matching a frustrating side effect with a simple, comforting food-based solution. Keep it handy for those days when you need a quick answer.
Common Side Effect | Foods That Can Help | Helpful Tips |
|---|---|---|
Nausea or Upset Stomach | Bland, easy-to-digest foods like crackers, toast, rice, and bananas. Ginger (tea, chews) and peppermint can also soothe the stomach. | Eat small, frequent meals instead of three large ones. Avoid greasy, spicy, or overly sweet foods that can trigger nausea. |
Fatigue | Lean proteins (chicken, fish, eggs, tofu) and complex carbohydrates (oats, quinoa, sweet potatoes). Iron-rich foods like spinach and lentils are also key. | Keep healthy, protein-rich snacks handy, like Greek yogurt or a handful of almonds. Staying hydrated is also crucial for energy. |
Taste Changes (Metallic or Bland) | Tart or citrus flavours like lemon, lime, and orange. Using plastic utensils can reduce a metallic taste. Herbs and spices can liven up bland food. | Experiment with different marinades and seasonings. If food tastes too sweet, add a squeeze of lemon. If it's too salty, a little sugar can help balance it. |
Mouth Sores or Dry Mouth | Soft, moist foods like smoothies, soups, scrambled eggs, and yogurt. Sucking on ice chips or sugar-free hard candies can help stimulate saliva. | Avoid crunchy, acidic, or spicy foods that can irritate a sore mouth. Use a straw for drinking liquids to bypass sensitive areas. |
Having these simple swaps in your back pocket can make a world of difference in your day-to-day comfort.
Practical Meal Ideas to Boost Well-Being
When you're exhausted, the last thing you want to do is tackle a complicated recipe. The goal here is maximum nutrition for minimal effort.
Here are a few simple but powerful ideas:
The Power Smoothie: Blend spinach, a scoop of protein powder, half a banana, a handful of berries, and almond milk. It’s a complete, easy-to-sip meal packed with vitamins, protein, and antioxidants.
Comforting Oatmeal: Fix a warm bowl of oatmeal with a swirl of almond butter for protein and healthy fats. Top it with sliced peaches or berries for natural sweetness and fibre.
Simple Chicken and Veggie Soup: Grab some low-sodium broth and toss in pre-cooked shredded chicken, frozen mixed vegetables, and a little pasta or rice. It's hydrating, gentle, and feels like a warm hug in a bowl.
Quick Scrambled Eggs: Whisk two eggs with a splash of milk and scramble them. Serve with a slice of whole-wheat toast for a fast, protein-packed meal that helps fight fatigue and rebuild tissues.
Remember, every small, nourishing choice you make is a deposit in your wellness bank. You are actively participating in your own healing journey, supporting your body with the kindness and fuel it truly deserves.
Thriving in Survivorship: Life After Treatment
When you ring that bell, take that final deep breath, and walk out of the treatment centre for the last time, the feeling is… surreal. There's this expectation that life will just snap back to how it was before. But the truth is, the journey doesn’t end there. It just shifts. Surviving triple positive breast cancer is one mountain climbed, and learning to thrive in survivorship is the beautiful, complex, and rewarding path that comes next.
This new phase is really about moving from patient back to person. It’s about figuring out who you are now, not just trying to be who you were before the diagnosis. It’s a time to give yourself so much grace, to accept that your story has a brand-new chapter, and to really embrace the incredible strength you’ve discovered along the way.
Navigating the Emotional Landscape of Survivorship
The end of treatment can bring a surprising, and honestly confusing, mix of emotions. Of course, there’s relief and gratitude. But for many of us, there's also a strange sense of unease. The safety net of frequent doctor visits is suddenly gone, and you’re left steering the ship on your own. Feeling this way is completely, 100% normal.
One of the biggest emotional hurdles is what many of us call "scanxiety." It's that intense wave of anxiety that crashes over you in the days or weeks leading up to a follow-up scan. Your mind starts racing with "what ifs," and every little ache or pain can feel like a giant red flag.
Here are a few ways to gently manage these feelings:
Acknowledge the Fear: Don't try to push it down or pretend it isn't there. Sometimes just saying it out loud helps. "I am scared about this scan." Naming the fear takes away some of its power over you.
Plan a Post-Scan Reward: Give yourself something to genuinely look forward to, no matter what the results are. It could be a coffee date with a friend, a quiet walk at your favourite park, or just an hour to dive into a good book. This shifts your focus from dread to anticipation.
Practice Mindful Breathing: When you feel that anxiety starting to peak, just close your eyes and focus on your breath. Inhale slowly for four counts, hold for four, and then exhale slowly for six. This simple exercise can calm your nervous system down in just a few minutes.
This period is also about finding your "new normal." Living with cancer changes you. Your priorities have likely shifted, your body feels different, and your perspective on what truly matters has probably been sharpened. My advice? Embrace this. It’s not about getting back to the "old you." It's about getting to know the resilient, incredible person you’ve become.
Building Your Support System for the Long Haul
Your support system was a lifeline during treatment, and it’s just as crucial in survivorship. The kind of support you need might change, though. Now, it's less about meals and rides to appointments and more about finding people who truly understand the long-term journey.
It's time to seek out connections that lift you up:
Fellow Survivors: Nobody "gets it" quite like someone who has walked a similar path. Online forums, local support groups, or that friend you made in the chemo suite can be an invaluable source of understanding.
Mental Health Professionals: Finding a therapist who specializes in oncology can be a game-changer. They can give you real tools to process the trauma of it all, manage the fear of recurrence, and help you redefine who you are now.
Honest Friends and Family: Lean on the people who let you be truly honest—the ones you can cry with, laugh with, and say, "Today is just a really hard day," without any judgment.
"Metastatic breast cancer has completely changed my outlook on life. It’s truly a blessing every day that we’re here... I want people to see that I’m out here living. I’m going through some things, but I’m living. I’m being a mom, I’m being a wife, I’m having a good time.” - Tiffany Kinkead
This powerful perspective shows that even when facing immense challenges, finding joy and purpose in the everyday is not just possible, but essential. Your diagnosis is part of your story, but it doesn't get to write the ending.
Finding Joy and Meaning in Your New Chapter
Survivorship is your personal invitation to live more intentionally. It's about finding joy not just in the big milestones, but in the small, quiet moments of an ordinary day. It’s about listening to your body, honouring its limits, and celebrating its incredible strength.
Think of this as a time of rediscovery. What brings you genuine joy? What have you always wanted to try? Maybe it’s painting, gardening, learning an instrument, or simply spending more quality time with the people you love. You’ve been given a unique lens to view the world through—one that sees the beauty in the present moment with incredible clarity.
This healing journey is so deeply personal. For more guidance on this path, you might find comfort in exploring [a guide to hope and healing in your breast cancer recovery](https://www.gracegritandpinkribbons.com/post/a-guide-to-hope-and-healing-in-your-breast-cancer-recovery), which offers more strategies for nurturing your spirit.
Your future isn’t defined by statistics or past struggles. It’s a blank canvas waiting for you to fill it with new colours, new experiences, and a profound appreciation for the life you fought so hard to live. You are more than a survivor; you are a thriver, standing on a foundation of unmatched grit and grace. A rich, meaningful life is waiting for you.
Your Questions Answered with Hope and Realism
When you get a triple positive breast cancer diagnosis, your mind is probably spinning with a million questions. It’s completely normal to feel a flood of "what ifs" and "what nows." This is a space to tackle some of the most common questions we hear, offering clear and realistic answers to help you feel more grounded.
Knowledge is a powerful tool against anxiety. Our goal is to untangle some of the confusion and give you the information you need to walk this path with more confidence.
Is Triple Positive Breast Cancer Better or Worse?
It's so tempting to want to label cancers as "good" or "bad," but it’s more helpful to see triple positive breast cancer as just... different. In fact, those "positives" are a huge advantage.
Think of it this way: instead of fighting an invisible enemy, your doctors know exactly what’s fuelling the cancer growth. They have three very specific targets—the estrogen receptor (ER), the progesterone receptor (PR), and the HER2 protein. This gives them a roadmap for a powerful, multi-pronged attack using targeted therapies and hormone therapy.
Yes, the treatment plan can feel intense. But having such clear targets often leads to very effective outcomes because we have specific, powerful weapons to fight it.
How Long Will I Be on Hormone Therapy?
This is a big one, and a question almost everyone asks. Hormone therapy (also called endocrine therapy) is a long-term game plan. It’s designed to drastically cut down the risk of the cancer coming back by blocking the hormones that fed it in the first place.
For most people, this means taking a daily pill for 5 to 10 years after the more aggressive treatments like chemo and surgery are done. The duration depends on:
Your age and whether you're pre- or post-menopausal.
The unique details of your tumour and your personal risk of recurrence.
How you’re managing the side effects. Your quality of life matters.
Your oncology team will work with you to map out a timeline that makes sense for you. It’s a long-term commitment, but it’s a crucial part of your survivorship plan.
Will I Lose My Hair During Treatment?
Hair loss is one of the most visible and emotionally tough side effects, but it’s not a given for everyone. It all comes down to your unique treatment plan.
The main culprit for significant hair loss is chemotherapy. While chemo is often part of the treatment for triple positive breast cancer, not every single patient will need it.
The other major treatments, like targeted therapies (Herceptin/trastuzumab) and hormone therapies, don’t usually cause the same kind of total hair loss. You might notice some thinning, but it’s typically far less dramatic. This is a perfect question to bring to your oncologist, who can give you a realistic idea of what to expect from your specific drug regimen.
"I was good that whole period off of Tamoxifen—no issues, no symptoms of breast cancer. I was back to being my normal self. I was probably even healthier because I was so focused on trying to make sure my body was in optimal state..." - Tiffany Kinkead
Tiffany's words really highlight how it’s possible to find your "normal" again, even during long-term treatment. It's all about finding that balance and focusing on your overall well-being as you move forward. Your journey is yours alone, and having open, honest conversations with your care team will make sure you feel prepared for every step of living with cancer and thriving beyond it.
At Grace Grit and Pink Ribbons, we believe in the power of shared stories and gentle encouragement. We are a dedicated online sanctuary offering heartfelt narratives and practical resources to guide you through every stage of your healing journey. Find your community and rediscover your strength with us.





Comments